Two Viable, Overlapping Models
Anecdote
Sports Team Doctor Calls the Shots
Portola Valley Physician Aims for Zero Pain
San Francisco Chronicle
October 7, 2000
Friends of Dr. Mark Sontag of Portola Valley, CA, like to joke that he's “a man for all seasons.”
A specialist in sports medicine and rehabilitation, Sontag is a team doctor for the San Francisco Giants, the San Jose Sharks, and the San Jose SaberCats, as well as is a consulting spinal physician for the Oakland Raiders and Menlo Colleges athletic programs. He has also treated players for the San Francisco 49ers.
In July 2000, Dr. Sontag and colleagues opened the Sports, Pain, and Rehabilitative Care Center in Menlo Park for the treatment of chronic and acute pain sufferers. Their patients are not elite athletes, but people with chronic pain syndrome who have undergone previous medical or surgical treatment with little or no relief.
Sontag has developed a theory about the levels of pain tolerance among athletes that now forms this center's treatment model.
Sontag, a certified physiatrist, said “neurological studies show that motion tends to block pain impulses to the brain.” In the case of some athletes, this enables them to perform at almost superhuman levels.
Sontag has established a pecking order of pain tolerance that puts hockey players at the highest pain threshold and baseball players at the lowest, with football players somewhere in the middle.
Eventually, he came to believe that there was a correlation between pain thresholds and how much continuous movement a particular sport demands of an injured athlete. “The more action, the less pain is likely to be felt, and I've observed that this applies not only to athletes but for others too.”
As examples, football has a relatively brief burst of action wrapped around lengthy strolls back to the huddle, timeouts and other and scheduled delays.
By comparison, hockey matches are 60 minutes of almost continuous action, while in baseball, players, may not do much for several innings at a time.
Introduction
In 1970, Princeton educated physiologist Irvin M. Korr, PhD, emphasized the importance of motion for life and health, stating (1):
What does human life consist of? What does man do?
Man does all the things that we see each other do. He moves, runs, works, plays tennis, builds buildings, paints pictures, makes music, makes love — to paraphrase the flower children, he makes love and war. He is creative. He teaches, learns, writes, educates, practices medicine, does surgery, and gives osteopathic manipulations.
If you look at these activities objectively, you will see that in all of them the body as a whole is moved or some part of the body is moved; and the common feature, the indispensable substratum, is the contraction of skeletal musculature. Human life is expressed through the contractile processes of striated muscle. Every aspect of human life is acted out by the body’s muscles and joints. Everything man does to express his aspirations and convictions can be perceived by others only through his bearing and demeanor and utterances, and these are composites of myriads of finely controlled motions.
Education itself is sometimes defined as a change in behavior and behavior is produced by muscles acting on joints.
Here then is an important conclusion which I think is implicit in the total osteopathic perspective: that the musculoskeletal system is the primary machinery of life. These are the body parts that act together to transmit and modify force and motion through which man acts out his life. But since machinery must be supplied with motor power in order to function, our concept of the primary biologic machinery should include its direction by the nervous system acting in response to the continual sensory input that reports what is going on in the outside environment and what is going on in the body itself; hence, the “neuromusculoskeletal” system.
If the musculoskeletal system and the nervous system that directs it comprise the primary machinery of life, then what is the function of all the rest of the bodily machinery with which medicine is so much concerned? As the title suggests, their function is entirely supportive. Their concern is with the care and maintenance of the primary machinery of life, which means supplying fuels and building materials, disposing of wastes and end products, taking care of the defense and repair and regeneration of components and in general maintaining regulation of the internal environment in which the cells of the primary machinery carry out their function.
The musculoskeletal system is the largest mass of the body and the main consumer. Muscles consume more energy, more rapidly and in wider ranges, than any other tissues in the body.
•••••••••
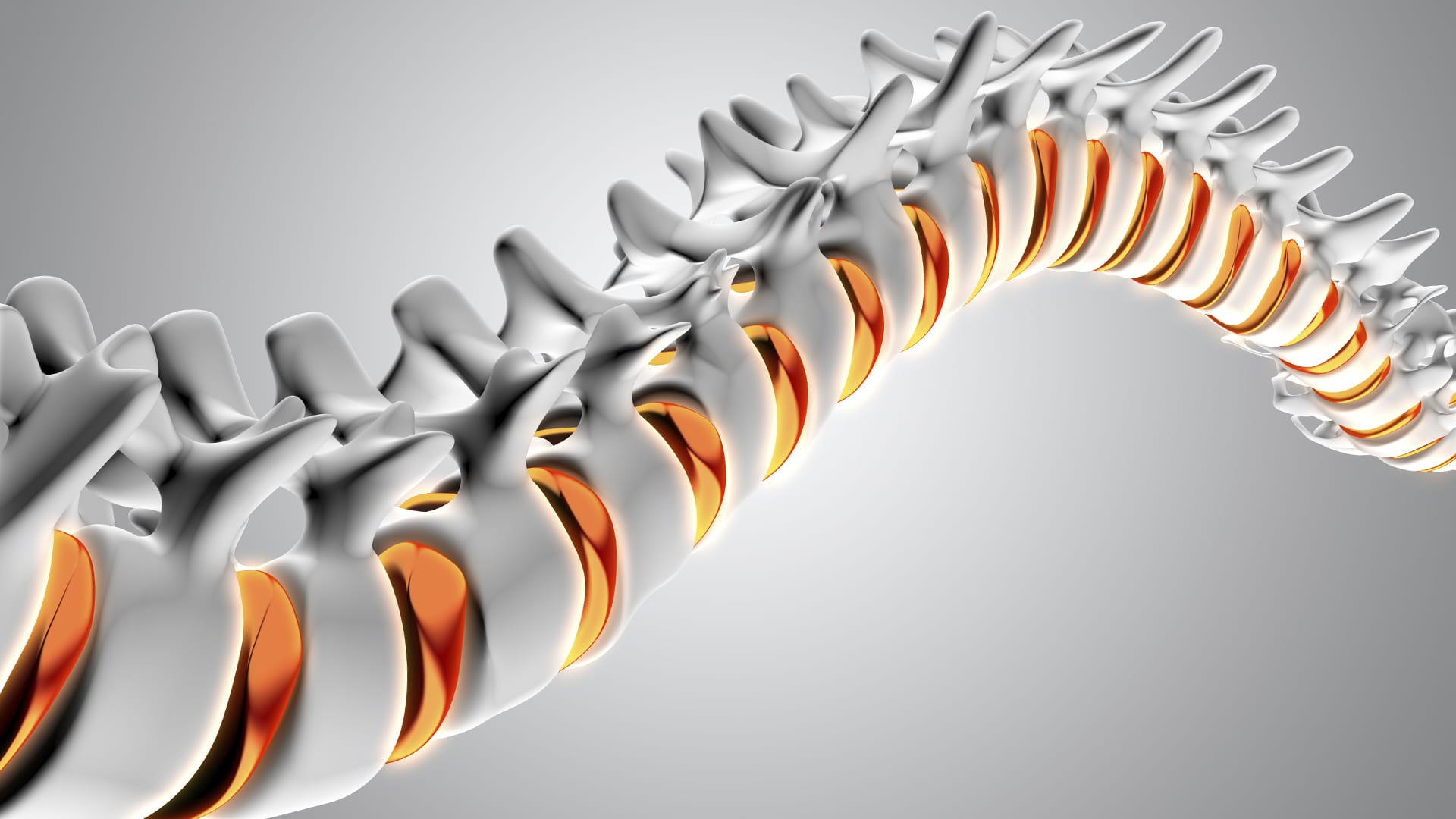
As noted by Dr. Korr, motion is critical for human life and its expression. The motion of the spine is dependent upon the integrity of the intervertebral disc. The intervertebral disc gives the spine its mobility (2). The intervertebral disc also acts as a shock absorber, and is primarily responsible for carrying all of the compressive loads to which the trunk is subjected (3).
The adult intervertebral disc is void of blood vessels (4, 5). Above and below each intervertebral disc is the vertebral body. The vertebral body is quite vascular (it has a well developed blood supply). Between the disc and the vertebral body is a porous cartilaginous end plate. Disc cell nutrition, health, water binding and hydrostatic properties are dependent upon motion. Deleterious consequences are inevitable following anything that impairs intervertebral disc motion.
(Picture from reference #6)
Reviews of pathology and the evolutionary basis for survivability links infection, inflammation, and excessive-harmful tissue fibrosis, resulting in impaired motion. Succinctly stated by James Cyriax, MD, in 1982 (7):
“The excessive reaction of tissues to an injury is conditioned by the overriding needs of a process designed to limit bacterial invasion. If there is to be only one pattern of response, it must be suited to the graver of the two possible traumas. However, elaborate preparation for preventing the spread of bacteria is not only pointless after an aseptic injury, but is so excessive as to prove harmful in itself. The principle on which the treatment of post-traumatic inflammation is based is that the reaction of the body to an injury unaccompanied by infection is always too great.”
Many others support this perspective (8, 9, 10, 11, 12, 13). In summary, for more than half a century, experts in pathology, physiology, orthopedics, sports injuries, and wound healing have suggested this model:
Inflammation is a paradox. Inflammation can directly kill pathogens. Inflammation also triggers a fibrous response that walls-off infection so that the pathogens are less likely to spread and kill the host. Without inflammation we would die of infection. All who are alive today had ancestors that could successfully initiate an inflammatory response, kill pathogens, and wall off the pathogens.
Infection can kill the young before they can reproduce. Hence, a strong inflammatory response is genetically selected, giving those with such a response a survivability advantage. Our ancestors genetically handed down these traits and we possess them. In a world prior to the availability of antibiotics, inflammation, with reactive walling-off fibrosis to contain pathogens, is desirable because it increases host survivability.
Infections were the primary cause of death for humans for millennias. Infections remained the primary cause of human death until very recent history, only a few decades ago.
Infection is not the only cause of inflammation. Inflammation is also triggered by trauma, excessive tissue stress, chemicals, and immunologic responses. Apparently, the body cannot distinguish the different causes of inflammation from each other, and they all trigger a fibrous response. “The resolution of inflammation in the body is fibrosis.”
This fibrosis response is necesasary when there is an infection, it is life-saving. However in an aseptic sterile injury or tissue stress, the fibrous response is excessive and it creates adverse mechanical deficits. These adverse mechanical deficits create tissue stiffness and limit the mobility of joints. These mechanical deficits impair local biomechanical function, affecting performance, generating pain, and accelerating degenerative changes.
For 40 years it has been understood that the structure primarily responsible for back pain, especially for chronic back pain, is the intervertebral disc (14, 15, 16, 17, 18, 19, 20). It is proposed that there is a connection between discogenic back pain and lack of intervertebral disc movement.
Model #1: Mechanics Influences Chemistry
The United States of America is plagued with chronic pain. Of the 238 million adults in America, approximately half of them have chronic daily pain (21). The conservative estimate of the direct costs and lost productivity resulting from this pain is up to $635 billion yearly (22).
Chronic pain affects every region of the body. Quantifying the anatomical regions for American’s chronic pain shows that the most significantly affected region is the lower back (23):
Hip Pain 07.1%
Finger Pain 07.6%
Shoulder Pain 09.0%
Neck Pain 15.1%
Severe Headache 16.1%
Knee Pain 19.5%
Lower-Back Pain 28.1%
Most pain is a chemical event. Inflammatory chemicals irritate pain nerves. The understanding of the inflammatory chemical nature of pain was awarded the Nobel Prize in Physiology or Medicine in 1982. In 2007, the journal Medical Hypothesis states (24):
“Every pain syndrome has an inflammatory profile consisting of the inflammatory mediators that are present in the pain syndrome.”
“The key to treatment of Pain Syndromes is an understanding of their inflammatory profile.”
“Our unifying theory or law of pain states: the origin of all pain is inflammation and the inflammatory response.”
“Irrespective of the type of pain whether it is acute or chronic pain, peripheral or central pain, nociceptive or neuropathic pain, the underlying origin is inflammation and the inflammatory response.”
“Activation of pain receptors, transmission and modulation of pain signals, neuro-plasticity and central sensitization are all one continuum of inflammation and the inflammatory response.”
“Irrespective of the characteristic of the pain, whether it is sharp, dull, aching, burning, stabbing, numbing or tingling, all pain arises from inflammation and the inflammatory response.”
The most common treatment of inflammatory pain is consumption of drugs, specifically non-steroidal anti-inflammatory drugs (NSAIDs). However, when these drugs (NSAIDs) are taken for chronic pain, there are many serious side effects. In 2003, the journal Spine states (25):
“Adverse reactions to non-steroidal anti-inflammatory (NSAID) medication have been well documented.”
“Gastrointestinal toxicity induced by NSAIDs is one of the most common serious adverse drug events in the industrialized world.”
“The newer COX-2-selective NSAIDs are less than perfect, so it is imperative that contraindications be respected.”
There is “insufficient evidence for the use of NSAIDs to manage chronic low back pain, although they may be somewhat effective for short-term symptomatic relief.”
In 2006, the journal Surgical Neurology states (26):
Blockage of the COX enzyme inhibits the conversion of arachidonic acid to the very pro-inflammatory prostaglandins that mediate the classic inflammatory response of pain.
“More than 70 million NSAID prescriptions are written each year, and 30 billion over-the-counter NSAID tablets are sold annually.”
“5% to 10% of the adult US population and approximately 14% of the elderly routinely use NSAIDs for pain control.”
Almost all patients who take the long-term NSAIDs will have gastric hemorrhage, 50% will have dyspepsia, 8% to 20% will have gastric ulceration, 3% of patients develop serious gastrointestinal side effects, which results in more than 100,000 hospitalizations, an estimated 16,500 deaths, and an annual cost to treat the complications that exceeds 1.5 billion dollars.
“NSAIDs are the most common cause of drug-related morbidity and mortality reported to the FDA and other regulatory agencies around the world.”
One author referred to the “chronic systemic use of NSAIDs to ‘carpet-bombing,’ with attendant collateral end-stage damage to human organs.”
Vert Mooney, MD (d. 2009), was a renowned and respected orthopedic surgeon. He was trained at Columbia University College of Physicians and Surgeons (Medical Doctor) and at the University of Pittsburgh (Orthopedic Surgeon).
Dr. Mooney was a founding member of the North American Spine Society (NASS), and he served as NASS President from 1987-1988. He also received the Lifetime Achievement Award in Lumbar Spine Research from the International Society for the Study of Lumbar Spine in 2008. His area of specialty was in advocating for non-surgical approaches to the management of acute and chronic lumbo-pelvic pain, and the promotion of interdisciplinary approaches to the prevention, diagnosis and treatment of lower back spinal problems.
In his 1986 Presidential Address of the International Society for the Study of the Lumbar Spine, Dr. Mooney made these comments in the journal Spine, in an article titled (16):
Where Is the Pain Coming From?
“In the United States in the decade from 1971 to 1981, the numbers of those individuals disabled from low-back pain grew at a rate 14 times that of the population growth. This is a greater growth of medical disability than any other. Yet this growth occurred in the very decade when there was an explosion of ergonomic knowledge, labor-saving mechanical assistance devices, and improved diagnostic equipment. We apparently could not find the source of pain.”
“Anatomically the motion segment of the back is made up of two synovial joints and a unique relatively avascular tissue found nowhere else in the body - the intervertebral disc. Is it possible for the disc to obey different rules of damage than the rest of the connective tissue of the musculoskeletal system?”
“Mechanical events can be translated into chemical events related to pain.”
“Mechanical activity has a great deal to do with the exchange of water and oxygen concentration” in the disc.
An important aspect of disc nutrition and health is the mechanical aspects of the disc related to the fluid mechanics.
The pumping action maintains the nutrition and biomechanical function of the intervertebral disc. Thus, “research substantiates the view that unchanging posture, as a result of constant pressure such as standing, sitting or lying, leads to an interruption of pressure-dependent transfer of liquid. Actually the human intervertebral disc lives because of movement.”
“The fluid content of the disc can be changed by mechanical activity.”
“In summary, what is the answer to the question of where is the pain coming from in the chronic low-back pain patient? I believe its source, ultimately, is in the disc. Basic studies and clinical experience suggest that mechanical therapy is the most rational approach to relief of this painful condition.”
This model supports this perspective:
- The intervertebral disc is the primary source of chronic low back pain.
- The disc in anatomically unique. Its lack of blood supply makes disc health dependent upon motion.
- All things that impair disc motion alter disc biochemistry. Altered disc biochemistry is inflammatory.
- Inflammatory disc biochemistry causes discogenic pain.
- Mechanical therapy that improves disc motion will mitigate disc inflammatory biochemistry, reducing pain.
- Anti-inflammatory drugs (NSAIDs), passive treatment modalities, and prolonged rest are not the solution to chronic low back pain.
Model #2: Motion “Closes” the Pain Gate
Melzack and Wall’s Gate Control Theory of Pain was originally published in the journal Brain in 1962 (27), and later updated and published in the journal Science in 1965 (28). Ronald Melzack, PhD, is a Canadian psychologist. Patrick Wall, MD (d. 2001), was a British neuroscientist and pain expert, as well as the first editor of the journal Pain. An oversimplified explanation of their Gate Control Theory of Pain is that the pain electrical signal to the cortical brain (small diameter afferents) can be inhibited by non-painful electrical signals arising from other sensory afferents (large diameter afferents). Representative reference book comments include:
The perception of pain is dependent upon the balance of activity in large (mechanoreceptor) and small (nociceptive) afferents. (29)
If large myelinated fibers (mechanoreceptors) were selectively stimulated, then normal “balance” of activity between large (mechanoreceptor) and small (nociceptive) fibers would be restored and the pain would be relieved. (29)
“Pain is not simply a direct product of the activity of nociceptive afferent fibers but is regulated by activity in other myelinated afferents that are not directly concerned with the transmission of nociceptive information.” (30)
“The idea that pain results from the balance of activity in nociceptive and nonnociceptive afferents was formulated in the 1960s and was called the gate control theory.” (30)
“Simply put, non-nociceptive afferents ‘close’ and nociceptive afferents ‘open’ a gate to the central transmission of noxious input.” (30)
“The balance of activity in small- and large-diameter fibers is important in pain transmission...” (30)
Melzack and Wall’s Gate Control Theory of Pain was reviewed and confirmed in 2002 in the British Journal of Anaesthesia in an article titled (31):
Gate Control Theory of Pain Stands the Test of Time
This article reiterates that the Gate Theory “has stood the test of time.” The electrical transmission and perception of pain is subject to modulation by non-nociceptive neurological electrical signals. These non-nociceptive neurological electrical signals emanate from large diameter nerve fibers, such as mechanoreceptors. Consequently, the author notes that pain can be modulated through 2 mechanisms (as noted above):
- Reducing excitation. This approach is commonly achieved by reducing inflammation.
- Increasing Inhibition. This approach is commonly achieved by improving mechanical function and mechanical afferentation, firing inhibitory large diameter mechanoreceptors.
The application of chiropractic spinal adjusting for pain control using
Melzack and Wall’s Gate Control Theory of Pain was first done by Canadian orthopedic surgeon Kirkaldy-Willis in 1985 (32). Dr. Kirdaldy-Willis notes:
“Spinal manipulation is essentially an assisted passive motion applied to the spinal apophyseal and sacroiliac joints.”
Melzack and Wall proposed the Gate Theory of Pain in 1965, and this theory has “withstood rigorous scientific scrutiny.”
“The central transmission of pain can be blocked by increased proprioceptive input.” Pain is facilitated by “lack of proprioceptive input.” This is why it is important for “early mobilization to control pain after musculoskeletal injury.”
The facet capsules are densely populated with mechanoreceptors. “Increased proprioceptive input in the form of spinal mobility tends to decrease the central transmission of pain from adjacent spinal structures by closing the gate. Any therapy which induces motion into articular structures will help inhibit pain transmission by this means.”
Stretching of facet joint capsules will fire capsular mechanoreceptors which will reflexly “inhibit facilitated motoneuron pools” which are responsible for the muscle spasms that commonly accompany low back pain.
In chronic cases, there is a shortening of periarticular connective tissues and intra-articular adhesions may form; manipulations [adjustments] can stretch or break these adhesions.
“In most cases of chronic low back pain, there is an initial increase in symptoms after the first few manipulations [probably as a result of breaking adhesions]. In almost all cases, however, this increase in pain is temporary and can be easily controlled by local application of ice.”
“However, the gain in mobility must be maintained during this period to prevent further adhesion formation.”
These patients were given a “two or three week regimen of daily spinal manipulations by an experienced chiropractor.”
“No patients were made worse by the manipulation, yet many experienced an increase in pain during the first week of treatment. Patients undergoing manipulative treatment must therefore be reassured that the initial discomfort is only temporary.”
“In our experience, anything less than two weeks of daily manipulation is inadequate for chronic low back pain patients.”
•••••••••
Conclusions
The study by Dickenson (31), published in the British Journal of Anaesthesia, notes that successful pain suppression should apply two approaches:
- Reducing excitation
- Increasing Inhibition
Both approaches are addressed with spinal manipulation. The increased segmental motion achieved with spinal manipulation will improve disc biochemistry, reducing inflammation and pain excitation.
The increased segmental motion achieved with spinal manipulation will also increase proprioception, leading to a neurological sequence of events that inhibits pain by “closing” the Pain Gate.
These models support the evidence showing that spinal manipulation is both safe and effective in the treatment of chronic low back pain.
REFERENCES
- Korr IM; The Sympathetic Nervous System as the Mediator Between the Somatic and Supportive Processes; The Collected Papers of Irvin M. Korr; The American Academy of Osteopathy; 1979; pp. 170-175.
- Turek SL; Orthopaedics: Principles and Their Applications; JB Lippincott Company; 1977; p. 1324.
- White AA, Panjabi MM; Clinical Biomechanics of the Spine; Second edition; JB Lippincott Company; 1990; p. 3.
- Harris RI, MacNab I; Structural changes in the lumbar intervertebral discs; their relationship to low back pain and sciatica; Journal of Bone and Joint Surgery, British; May 1954;36-B(2):304-22.
- Hassler O; The human intervertebral disc. A micro-angiographical study on its vascular supply at various ages; ACTA Ortho Scand; 1969; 40(6):765-72.
- Kapandji IA; The Physiology of the Joints; Volume 3; The Trunk and the Vertebral Column; Churchill Livingstone; 1974.
- Cyriax, James; Textbook of Orthopaedic Medicine, Diagnosis of Soft Tissue Lesions; Bailliere Tindall; Volume 1; eighth edition; 1982.
- Boyd W; PATHOLOGY: Structure and Function in Disease; Eighth Edition; Lea & Febiger; Philadelphia; 1970.
- Anderson WAD, Scotti TM; Synopsis of Pathology; Ninth Edition; The CV Mosby Company; 1976.
- Robbins SL, Cotran RS; PATHOLOGIC BASIS OF DISEASE; Second Edition; WB Saunders Company; Philadelphia; 1979.
- Roy, Steven; Irvin, Richard; Sports Medicine: Prevention, Evaluation, Management, and Rehabilitation; Prentice-Hall; 1983.
- Guyton A; Textbook of Medical Physiology; Saunders; 1986.
- Cohen, Kelman; Diegelmann, Robert F; Lindbald, William J; Wound Healing, Biochemical & Clinical Aspects; WB Saunders; 1992.
- Nachemson AL; The Lumbar Spine, an Orthopedic Challenge; Spine; Volume 1, Number 1, March 1976, pp. 59-71.
- Bogduk N, Tynan W, Wilson AS; The nerve supply to the human lumbar intervertebral discs; Journal of Anatomy; 1981; Vol. 132; No. 1; pp. 39-56.
- Mooney V; Where Is the Pain Coming From?; Spine; Vol. 12; No. 8; 1987; pp. 754-759.
- Kuslich S, Ulstrom C, Michael C; The Tissue Origin of Low Back Pain and Sciatica: A Report of Pain Response to Tissue Stimulation During Operations on the Lumbar Spine Using Local Anesthesia; Orthopedic Clinics of North America; Vol. 22; No. 2; April 1991; pp. 181-187.
- Ozawa T, Ohtori S, Inoue G, Aoki Y, Moriya H, Takahashi; The Degenerated Lumbar Intervertebral Disc is Innervated Primarily by Peptide-Containing Sensory Nerve Fibers in Humans; Spine Volume 31; Number 21; October 1, 2006; pp. 2418-2422.
- DePalma MJ, Ketchum JM, Saullo T; What is the source of chronic low back pain and does age play a role?; Pain Medicine; Feb 2011; Vol. 12; No. 2; pp. 224-233.
- Izzo R, Popolizio T, D’Aprile P, Muto M; Spine Pain; European Journal of Radiology; May 2015; Vol. 84; pp. 746–756.
- Foreman J; A Nation in Pain, Healing Our Biggest Health Problem; Oxford University Press; 2014.
- Pho, K; USA TODAY, The Forum; September 19, 2011; pg. 9A.
- Wang S; Why Does Chronic Pain Hurt Some People More?; Wall Street Journal; October 7, 2013.
- Sota Omoigui S; The biochemical origin of pain: The origin of all pain is inflammation and the inflammatory response: Inflammatory profile of pain syndromes; Medical Hypothesis; 2007, Vol. 69; pp. 1169–1178.
- Giles LGF;Reinhold Muller R; Chronic Spinal Pain: A Randomized Clinical Trial Comparing Medication, Acupuncture, and Spinal Manipulation; Spine; July 15, 2003; 28(14):1490-1502.
- Maroon JC, Bost JW; Omega-3 Fatty acids (fish oil) as an anti-inflammatory: an alternative to nonsteroidal anti-inflammatory drugs for discogenic pain; Surgical Neurology; 65 (April 2006); pp. 326–331.
- Melzack R, Wall PD; On the nature of cutaneous sensory mechanisms; Brain; June 1962; 85:331-56.
- Melzack R, Wall PD; Pain mechanisms: a new theory; Science; November 19, 1965; 150(3699):971-9.
- John Nolte, The Human Brain; Mosby Year Book, 1993.
- Eric Kandel, James Schwartz, Thomas Jessell, Principles of Neural Science. McGraw-Hill, 2000.
- Dickenson AH; Gate Control Theory of pain stands the test of time; British Journal of Anaesthesia, 88, No. 6, June 2002, pp. 755-757.
- Kirkaldy-Willis WH, Cassidy JD; Spinal Manipulation in the Treatment of Low back Pain; Canadian Family Physician; March 1985; Vol. 31; pp. 535-540.