The public press and indexed journals have claimed that chiropractic adjustments to the cervical spine can injure the vertebral artery. Students in Chiropractic College are also taught about the vertebral artery injury risk. Specifically, in college, chiropractic students are taught about:
- The anatomy of the cervical spine and of the vertebral artery.
- The manipulative maneuvers that theoretically would have the greatest risk of injuring the vertebral artery.
- The signs and symptoms of a person who is having vascular compromise of their vertebral artery.
The anatomy of the cervical spine and of the vertebral artery
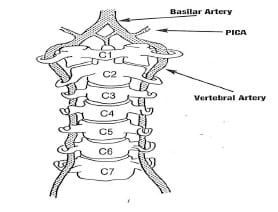
The brain is supplied by blood from two arterial sources: the paired internal carotid arteries and the paired vertebral arteries. The blood supply to the brain from the carotid arteries is referred to as the anterior circulation to the brain. The blood supply to brain from the vertebral arteries is referred to as the posterior circulation to the brain. The vertebral arteries are noted in the above drawing (reference 1).
The vertebral arteries are the main blood supply to the brain stem (where the cranial nerves originate), to the cerebellum (for coordination of movements) and to the occipital lobe of the brain (for vision). Consequently, interruption of blood flow through the vertebral arteries tends to give rise to signs and symptoms that are associated with these anatomical regions. These signs and symptoms are elaborated upon below.
The vertebral arteries are exceptionally unique: they ascend to the brain through an opening, a foramen, in the transverse process of the cervical vertebrae. This opening is called the foramen transversarium. The foramen transversarium exists in the cervical vertebrae C6-C1. The vertebral arteries ascend in the foramen transversarium before entering the skull through the foramen magnum. After entering the skull, the paired vertebral arteries merge to become the singular basilar artery (drawing from reference 1).
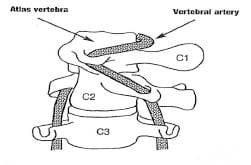
The atlas-axis (C1-C2) vertebral articulation of the cervical spine is mechanically unique. It is designed for the function of rotational motion. When one maximally turns one’s head, approximately 55% of that motion occurs at the atlas-axis articulation. The vertebral artery in the foramen transversarium between the atlas and axis must accommodate this rotational motion. This places the vertebral artery at increased risk of tractional types of stress and potential injury as a consequence of a variety of upper cervical spine mechanical loads.
The potential tractional injury to the vertebral artery is a dissection, and usually referred to as vertebral artery dissection, or VAD.
Right cervical spine (head) rotation, showing the tension on the left vertebral artery between the atlas and axis (drawing from reference 1).
The manipulative maneuvers that theoretically would have the greatest risk of injuring the vertebral artery
When there is a vertebral artery vascular event, imaging and pathology have noted vertebral artery dissection. The most plausible explanation for the vertebral artery dissection is a stretching injury. As noted above, over 50% of cervical spine rotation occurs at a single articulation, Atlas (C1) – Axis (C2). As depicted in the drawing above, C1-C2 rotation would stretch the vertebral artery.
Consequently, students in Chiropractic College are taught not to apply a rotational manipulative thrust of C1 on C2. Furthermore, biomechanical studies indicate that the vertebral artery will experience additional tractional stress if the upper cervical spine is in extension. It is emphasized to students in Chiropractic College to not use the combination of C1—C2 extension—rotation—thrust manipulation (adjustments).
The signs and symptoms of a person who is having vascular compromise of their vertebral artery
Signs and symptoms that would warn of a possible vertebral artery dissection with ischemia are often summarized as the 5 Ds And the 3 Ns (1):
Dizziness (vertigo, light-headedness)
Drop attacks
Diplopia (or other visual problems)
Dysarthria [Speech Disorder]
Dysphagia [Difficult or Painful Swallowing]
Ataxia of gait (Hemiparesis)
Nausea (possibly with vomiting)
Nystagmus
Numbness (hemianesthesia)
A history that would warn of a possible acute vertebral artery dissection with ischemia involves a sudden onset of severe head and/or neck pain, which is like no other pain the patient has previously suffered. This is especially important if the patient can isolate the pain to the suboccipital region (1).
Background
Cervical arterial dissection is one of the main causes of ischemic stroke in young adults. Cervical arterial dissections can be categorized as traumatic or spontaneous. The primary cause of posttraumatic cervical artery dissections is motor vehicle collisions (whiplash trauma) (2, 3).
According to a review of the literature by Alan Terrett (1), a number of non-manipulative mechanical events have been linked to vertebral artery dissections. These mechanical events usually involve rotation and/or extension, and include:
Childbirth
By Surgeon or Anesthetist During Surgery
Calisthenics, Athletics, Fitness Exercise
Yoga
Overhead Work, Painting a Wall
Hanging Out the Washing
Neck Extension during Radiography
Neck Extension for a Bleeding Nose
Turning the Head while Driving a Vehicle
Tonic Clonic Convulsive Seizure
Amusement Park Ride
Protracted Dental Work
Archery
Sneezing/Nose Blowing/Coughing
Wrestling
Emergency Resuscitation
Star Gazing, Watching Aircraft
Sleeping Position
Swimming
Break Dancing
Football
Beauty Parlor Stroke, Sitting in a Barber's Chair
Tai Chi
Sexual Intercourse
In another article by Alan Terrett (4), the published literature was reviewed pertaining to the incidence of reported adverse events associated with chiropractic spinal adjusting (manipulation). Astonishingly, his results revealed that in many of the published adverse events ascribed to chiropractic manipulation, they were in fact, not associated with chiropractic in any manner. Apparently, the authors of the articles assumed “chiropractic” and “manipulation” were synonyms. When untrained laypersons or physicians performed a manipulation resulting in a reported adverse event, authors would claim that the manipulation was performed by a chiropractor. The list of discovered manipulators included:
A Blind Masseur
An Indian Barber
A Wife
A Kung-Fu Practitioner
Self Manipulation
Often the manipulation was performed by a medical doctor, an osteopath, a naturopath, or a physical therapist.
Dr. Terrett concluded:
“This study reveals that the words chiropractic and chiropractor commonly appear in the literature to describe spinal manipulative therapy, or practitioner of spinal manipulative therapy, in association with iatrogenic complications, regardless of the presence or absence of professional training of the practitioner involved.”
“The words chiropractic and chiropractor have been incorrectly used in numerous publications dealing with spinal manipulative therapy injury by medical authors, respected medical journals and medical organizations.”
“In many cases, this is not accidental; the authors had access to original reports that identified the practitioner involved as a non-chiropractor. The true incidence of such reporting cannot be determined.”
“Such reporting adversely affects the reader's opinion of chiropractic and chiropractors.”
“It has been clearly demonstrated that the literature of medical organizations, medical authors and respected, peer-reviewed, indexed journals have, on numerous occasions, misrepresented the facts regarding the identity of a practitioner of manual therapy associated with patient injury.”
“Such biased reporting must influence the perception of chiropractic held by the reader, especially when cases of death, tetraplegia and neurological deficit are incorrectly reported as having been caused by chiropractic.”
“Because of the unwarranted negative opinion generated in medical readers and the lay public alike, erroneous reporting is likely to result in hesitancy to refer to and underutilization of a mode of health care delivery.”
Following Dr. Terrett’s lead, other authors have watched the indexed literature and continue to note that when an untrained individual injures a patient using spinal manipulation, it is often reported as having been done by a chiropractor. Examples include:
5) Weban A, Beck J, Raabe A, Dettmann E. Seifert V; Misuse of the terms chiropractic and chiropractor J Neurol Neurosurg Psychiatry. 2004 May; 75(5): 794.
“I am attempting to clarify this important difference between a chiropractor and chiropractitioner because there is the potential to create confusion such that the injury reported by Beck et al could be incorrectly attributed to a chiropractor as compared with a chiropractitioner (lay medical practitioner). In fact, unfortunately, this has already happened. A brief review of Dr. Beck’s case report, by a BMJ editor, inappropriately uses the title ‘chiropractic causes CSF leak’ and suggests the care provider was a chiropractor.”
6) Weban A; Inappropriate use of the title 'chiropractor' and term 'chiropractic manipulation' in the peer-reviewed biomedical literature. Chiropractic and Osteopathy; 2006 Aug 22;14:16.
“The results of this year-long prospective review suggests that the words 'chiropractor' and 'chiropractic manipulation' are often used inappropriately by European biomedical researchers when reporting apparent associations between cervical spine manipulation and symptoms suggestive of traumatic injury. Furthermore, in those cases reported here, the spurious use of terminology seems to have passed through the peer-review process without correction. Additionally, these findings provide further preliminary evidence, beyond that already provided by Terrett, that the inappropriate use of the title 'chiropractor' and term 'chiropractic manipulation' may be a significant source of over-reporting of the link between the care provided by chiropractors and injury.”
In 2002, Dr. Scott Haldeman from the Department of Neurology, University of California, Irvine, and colleagues, published a study titled (7):
“Unpredictability of cerebrovascular ischemia associated with cervical spine manipulation therapy: a review of sixty-four cases after cervical spine manipulation”
The study, published in Spine, was a retrospective review of 64 medicolegal records describing cerebrovascular ischemia after cervical spine manipulation. The authors note, that up to 2002, only about “117 cases of post-manipulation cerebrovascular ischemia have been reported in the English language literature.”
The authors further indicate that proposed risk factors for cerebrovascular ischemia secondary to spinal manipulation include age, gender, migraine headaches, hypertension, diabetes, birth control pills, cervical spondylosis, and smoking, and that it is often assumed that these complications may be avoided by clinically screening patients and by pre-manipulation positioning of the head and neck to evaluate the patency of the vertebral arteries. However, after an extensive review, these authors conclude:
“This study was unable to identify factors from the clinical history and physical examination of the patient that would assist a physician attempting to isolate the patient at risk of cerebral ischemia after cervical manipulation.”
“Cerebrovascular accidents after manipulation appear to be unpredictable and should be considered an inherent, idiosyncratic, and rare complication of this treatment approach.”
In 2008, Dr. David Cassidy and colleagues published the most comprehensive study to date pertaining to the risk of vertebral artery dissection as related to chiropractic cervical spine manipulation (8). The article was published in Spine, and titled:
“Risk of Vertebrobasilar Stroke and Chiropractic Care:
Results of a Population-Based Case-Control and Case-Crossover Study”
Key points from this article include:
“Vertebrobasilar artery stroke is a rare event in the population.”
“We found no evidence of excess risk of vertebral artery stroke associated chiropractic care.”
“Neck pain and headache are common symptoms of vertebral artery dissection, which commonly precedes vertebral artery stroke.”
“The increased risks of vertebral artery stroke associated with chiropractic and primary care physicians visits is likely due to patients with headache and neck pain from vertebral artery dissection seeking care before their stroke.”
“Because patients with vertebrobasilar artery dissection commonly present with headache and neck pain, it is possible that patients seek chiropractic care for these symptoms and that the subsequent vertebral artery stroke occurs spontaneously, implying that the association between chiropractic care and vertebral artery stroke is not causal.”
“Since it is unlikely that primary care physicians cause stroke while caring for these patients, we can assume that the observed association between recent primary care physician care and vertebral artery stroke represents the background risk associated with patients seeking care for dissection-related symptoms leading to vertebral artery stroke. Because the association between chiropractic visits and vertebral artery stroke is not greater than the association between primary care physicians visits and vertebral artery stroke, there is no excess risk of vertebral artery stroke from chiropractic care.”
“Our results suggest that the association between chiropractic care and vertebral artery stroke found in previous studies is likely explained by presenting symptoms attributable to vertebral artery dissection.”
In August of 2010, Donald Murphy published an article in the journal Chiropractic and Osteopathy, titled (9):
Current understanding of the relationship between cervical manipulation and stroke:
What does it mean for the chiropractic profession?
In this article, Dr. Murphy states:
“The understanding of the relationship between cervical manipulative therapy (CMT) and vertebral artery dissection and stroke (VADS) has evolved considerably over the years.”
“In the beginning the relationship was seen as simple cause-effect, in which CMT was seen to cause VADS in certain susceptible individuals. This was perceived as extremely rare by chiropractic physicians, but as far more common by neurologists and others.”
“Recent evidence has clarified the relationship considerably, and suggests that the relationship is not causal, but that patients with VADS often have initial symptoms which cause them to seek care from a chiropractic physician and have a stroke some time after, independent of the chiropractic visit.”
In January of 2011, the Journal of Manipulative and Physiological Therapeutics published a population-based case series using administrative health care records of all Ontario, CAN, residents hospitalized with vertebral artery stroke between April 1, 1993, and March 31, 2002, titled (10):
“A population-based case-series of Ontario patients who develop a vertebrobasilar artery stroke after seeing a chiropractor”
These authors note:
“The current evidence suggests that association between chiropractic care and vertebrobasilar artery (VBA) stroke is not causal. Rather, recent epidemiological studies suggest that it is coincidental and reflects the natural history of the disorder.”
“Because neck pain and headaches are symptoms that commonly precede the onset of a VBA stroke, these patients might seek chiropractic care while their stroke is in evolution.”
Also in January, The Open Neurology Journal published an “open access” editorial by Dean Smith and Gregory Cramer, titled (11):
“Spinal Manipulation is Not an Emerging Risk Factor for Stroke Nor is it Major Head/Neck Trauma. Don't Just Read the Abstract!”
Dean L. Smith is Clinical Faculty, Department of Kinesiology and Health, Miami University, Oxford, Ohio, and Gregory D. Cramer is Professor and Dean of Research, National University of Health Sciences, Lombard, Illinois. Their editorial includes:
We would like to address two points in this letter:
1) The current best-evidence indicates no causal relationship between spinal manipulation (‘chiropractic maneuver’ in the paper) and vertebrobasilar artery (VBA) stroke, and,
2) Spinal manipulation or ‘chiropractic maneuvers’ are not major head/neck trauma as suggested in abstract of this article.
“First, evidence is mounting that the association between spinal manipulation and stroke is coincidental rather than causal and reflects the natural history of the disorder.” (ref 10)
“The largest population-based study to date was conducted by Cassidy et al. and included all vertebrobasilar artery (VBA) strokes in Ontario, Canada over a period of 9 years. The authors found no evidence of excess risk (i.e. no risk) of VBA stroke associated with chiropractic care.” (ref 8)
“The prevailing hypothesis is that patients with vertebral artery dissections often have initial symptoms that cause them to seek care from a chiropractic or medical physician and the stroke is independent of their visit.” (ref 8, 9, 10)
The “population based study provides higher quality evidence than previous case reports, case series, and physician surveys frequently referenced when discussing spinal manipulation in this context.”
“If anything, the latest scientific evidence questions whether spinal manipulation is a risk factor at all for cervical artery dissection.”
“Chiropractic spinal manipulations may very well be a demerging risk factor for stroke since there may not be any risk.” (ref 8)
“The evidence, albeit limited to date, suggests that spinal manipulative treatments produce stretches of the vertebral artery that are much smaller than those that are produced during normal everyday movements, and thus they appear harmless.”
“Spinal manipulations delivered by licensed chiropractors do not fulfill the criteria for major trauma and should not be considered major trauma.”
In January of this year (2012), a study published in the Journal of Orthopaedic & Sports Physical Therapy, titled (12):
Upper Cervical and Upper Thoracic Thrust Manipulation Versus Nonthrust Mobilization in Patients With Mechanical Neck Pain:
A Multicenter Randomized Clinical Trial
All seven of the authors are physical therapists. The study was a randomized clinical trial to compare the short-term effects of upper cervical (C1-2) and upper thoracic (T1-2) high-velocity low-amplitude (HVLA) thrust manipulation to nonthrust mobilization in patients with neck pain. The authors note:
“The patients with mechanical neck pain who received the combination of upper cervical and upper thoracic HVLA thrust manipulation experienced significantly greater reductions in disability (50.5%) and pain (58.5%) than those of the nonthrust mobilization group (12.8% and 12.6%, respectively) following treatment.”
“The combination of upper cervical and upper thoracic HVLA thrust manipulation is appreciably more effective in the short term than nonthrust mobilization in patients with mechanical neck pain.”
Important for this discussion is the nature of the C1-C2 manipulations. From the picture and description, the C1-C2 manipulation appeared to be a rotational lateral flexion maneuver contacting the posterior arch of C1. For each manipulation the therapist tried to elicit an audible release, but tried to do so no more than twice. The descriptions and photographs appeared to show a standard joint cavitation rotational maneuver. In defending their use of such a maneuver, the authors state:
“The most recent and robust evidence for the risk of vertebrobasilar stroke and cervical HVLA thrust manipulation comes from the case control study by Cassidy et al. Contrary to traditionally held views, Cassidy et al (ref 8) found no evidence of excess risk of vertebrobasilar stroke associated with cervical HVLA thrust manipulation as compared to primary medical physician care. Moreover, a recent systematic review concluded that there has been no strong evidence linking the occurrence of serious adverse events with the use of cervical manipulation or mobilization in adults with neck pain.”
The biomechanics of cervical spine manipulation and vertebral artery stress is important. The world leader on this type of biomechanical assessment is Walter Herzog, PhD, from the University of Calgary, CAN. In April of this year (2012), Dr. Herzog and colleagues published a study in the Journal of Electromyography and Kinesiology titled (13):
Vertebral artery strains during high-speed, low amplitude cervical spinal manipulation
Dr. Herzog notes that spinal manipulative therapy (SMT) is recognized as an effective treatment modality for many back, neck and musculoskeletal problems. Yet, one of the major issues of the use of SMT is its safety, especially with regards to neck manipulation and the risk of stroke. It has been assumed [wrongly as per this study] that the vertebral artery (VA) experiences considerable stretch during extension and rotation of the neck, which may lead to occlusions and damage to the VA, predisposing the patient to stroke. Therefore, this study presents the first ever data on the mechanics between C2/C1 during cervical SMT performed by chiropractic clinicians.
The authors compared the results of human VA strains during high-speed, low-amplitude SMTs administered by qualified chiropractic clinicians and compared them to the strains encountered during full range of motion (ROM) tests. They used a total of 3,034 segment strains obtained during SMTs and 2,380 segment strains obtained during full ROM testing, making this is an extensive study.
Dr. Herzog and colleagues conclude:
“VA strains obtained during SMT are significantly smaller than those obtained during diagnostic and range of motion testing, and are much smaller than failure strains.”
“We conclude from this work that cervical SMT performed by trained clinicians does not appear to place undue strain on VA, and thus does not seem to be a factor in vertebro-basilar injuries.”
“In summary, the maximal strain values for the ROM testing at each segmental level were always greater than the corresponding strain values for the SMTs, suggesting that neck SMTs impose less stretch than turning your head, or extending your neck while looking up at the sky.”
“Therefore, based on the mechanical tests performed here, one should be able to conclude that stretching of VA during neck SMTs does not cause any damage of the VAs.”
“The VA is never really strained during spinal manipulative treatments but that the VA is merely taking up slack as the neck and head are moved during SMT, but that there is no stress and thus no possibility for microstructural damage.”
“The results from this study demonstrate that average and maximal VA strains during high-speed low-amplitude cervical spinal manipulation are substantially less than the strains that can be achieved during ROM testing for all vertebral artery segments.”
“We conclude that cervical spinal manipulations, as tested here, are safe from a mechanical point of view for normal, healthy VA.”
SUMMARY
Chiropractic students and chiropractors are extensively trained in the anatomy and biomechanics of the upper cervical spine. They are also extensively trained in the science and art of spinal adjusting (specific directional manipulation). The review presented here suggests:
1) Chiropractic manipulation may pose no risk of abnormal stretch to the vertebral artery.
2) Vertebral artery injury ascribed to chiropractic manipulation in the indexed literature is often inappropriate as the actual manipulation was done by an untrained layperson or untrained healthcare provider.
3) The symptoms associated with spontaneous vertebral artery dissection may bring the patient into chiropractic offices.
Chiropractors are extensively trained in understanding the 5 Ds And the 3 Ns that would suggest the possibility of a vertebral artery dissection, and the need for an immediate emergency referral. The best-published studies indicate that chiropractic spinal manipulation is both safe and effective.
REFERENCES
- Terrett AGJ; Current Concepts in Vertebrovascular Complications Following Spinal Manipulation; Second Edition; NCMIC Group, 2001.
- Hauser V, Zangger P, Winter Y, Oertel W, Kesselrin J; Late Sequelae of Whiplash Injury with Dissection of Cervical Arteries; European Neurology; August 18, 2010, Vol. 64, No. 4, pp. 214–218.
- Haneline M, Triano J. Cervical artery dissection. A comparison of highly dynamic mechanisms: manipulation versus motor vehicle collision. Journal of Manipulative Physiological Therapeutics. 2005 Jan;28(1):57-63.
- Terrett AG; Misuse of the literature by medical authors in discussing spinal manipulative therapy injury; Journal of Manipulative and Physiological Therapeutics; 1995 May;18(4):203-10.
- Weban A, Beck J, Raabe A, Dettmann E. Seifert V; Misuse of the terms chiropractic and chiropractor J Neurol Neurosurg Psychiatry. 2004 May; 75(5): 794.
- Weban A; Inappropriate use of the title 'chiropractor' and term 'chiropractic manipulation' in the peer-reviewed biomedical literature. Chiropractic and Osteopathy; 2006 Aug 22;14:16.
- Haldeman S, Kohlbeck FJ, McGregor M; Unpredictability of cerebrovascular ischemia associated with cervical spine manipulation therapy: a review of sixty-four cases after cervical spine manipulation; Spine; 2002 Jan 1;27(1):49-55.
- Cassidy, J David DC, PhD; Boyle, Eleanor PhD; Côté, Pierre DC, PhD; He, Yaohua MD, PhD; Hogg-Johnson, Sheilah PhD; Silver, Frank L. MD; Bondy, Susan J. PhD; Risk of Vertebrobasilar Stroke and Chiropractic Care: Results of a Population-Based Case-Control and Case-Crossover Study; Spine; Volume 33(4S), February 15, 2008 pp. S176-S183.
- Murphy DR; Current understanding of the relationship between cervical manipulation and stroke: what does it mean for the chiropractic profession?; Chiropractic and Osteopathy; 2010 Aug 3;18:22.
- Choi S, Boyle E, Cote P, Cassidy JD. A population-based case-series of Ontario patients who develop a vertebrobasilar artery stroke after seeing a chiropractor. J Manipulative Physiol Ther 2011; 34(1): 15-22.
- Smith DL, Cramer GC; LETTER TO THE EDITOR: Spinal Manipulation is Not an Emerging Risk Factor for Stroke Nor is it Major Head/Neck Trauma. Don't Just Read the Abstract!; The Open Neurology Journal, 2011, 5, 46-47
- Dunning JR, Cleland JA, Waldrop MA, Arnot C, Young I, Turner M, Sigurdsson G; Upper Cervical and Upper Thoracic Thrust Manipulation Versus Nonthrust Mobilization in Patients With Mechanical Neck Pain: A Multicenter Randomized Clinical Trial; Journal of Orthopaedic & Sports Physical Therapy; January 2012; Volume 42; Number 1; pp. 5-18.
- Herzog W, Leonard TR, Symons B, Tang C, Wuest S; Vertebral artery strains during high-speed, low amplitude cervical spinal manipulation; Journal of Electromyography and Kinesiology; April 5, 2012 [epub].



